Caption Health
Helping non-specialists deliver echocardiograms in any setting
In a previous article, Zachary Bogue and I outlined the emergence of a new category of startup at the intersection of technology and medicine: TechMed. These companies leverage artificial intelligence, machine learning, computer vision, and novel sensor technologies to deliver breakthroughs in clinical insights and care. They start not with a particular device, but with unique, proprietary datasets and sophisticated algorithms that can transform every stage of the patient journey.
In this sequel to that article, I will double-click on one of the most exciting and transformative aspects of the TechMed revolution: the rise of Somatic AI. I’ll explain what it is, how it differs from other buzzed-about forms of AI, and why it represents an unprecedented opportunity for startups, investors, and the future of care delivery.
Somatic AI: healthcare’s new ‘little black bag’
Much of the fervor in tech investing over the past two years has centered on Generative AI — large language models like GPT‑4 that can produce text, images, and code at levels that closely approximate human capabilities. In parallel, a class of Enterprise AI applications has gained traction by streamlining knowledge work in domains like law, finance, and customer service. Both approaches have made inroads into healthcare, powering use cases like clinical documentation and revenue cycle management.
However, the most profound wave of AI-driven transformation in medicine has yet to hit the mainstream. I call it Somatic AI — a new generation of AI systems purpose-built to understand and interact with the human body. Somatic AI combines insights from medical imaging, digital biomarkers, real-time sensing, and other patient data modalities to build high-resolution computational models of individual anatomy and physiology. Fed by a continuous flow of multi-modal data — a data river — these models serve as the foundation for a wide array of breakthrough clinical applications, from AI-guided surgical navigation and autonomous robotic procedures to intelligent patient monitoring and real-time clinical decision support.
The core enabling technologies behind Somatic AI — computer vision, sensor fusion, GPU-accelerated computation — are frequently birthed not in the medical device industry, but in other domains like autonomous vehicles, industrial robotics, and consumer electronics. In that sense, Somatic AI represents a second wave of artificial intelligence in healthcare, building on but distinct from the initial forays focused on digital health workflows and back-end operations.
The potential of Somatic AI to democratize early disease detection and intervention is already being realized through wearable devices like the Apple Watch. In one recent example, a friend of mine woke up to an alert from his Apple Watch indicating that his heart was in atrial fibrillation (AFib). This early warning allowed him to seek timely medical attention and potentially avoid serious complications. As Somatic AI advances, we can expect even more proactive and personalized insights to be delivered directly to patients and their care teams.
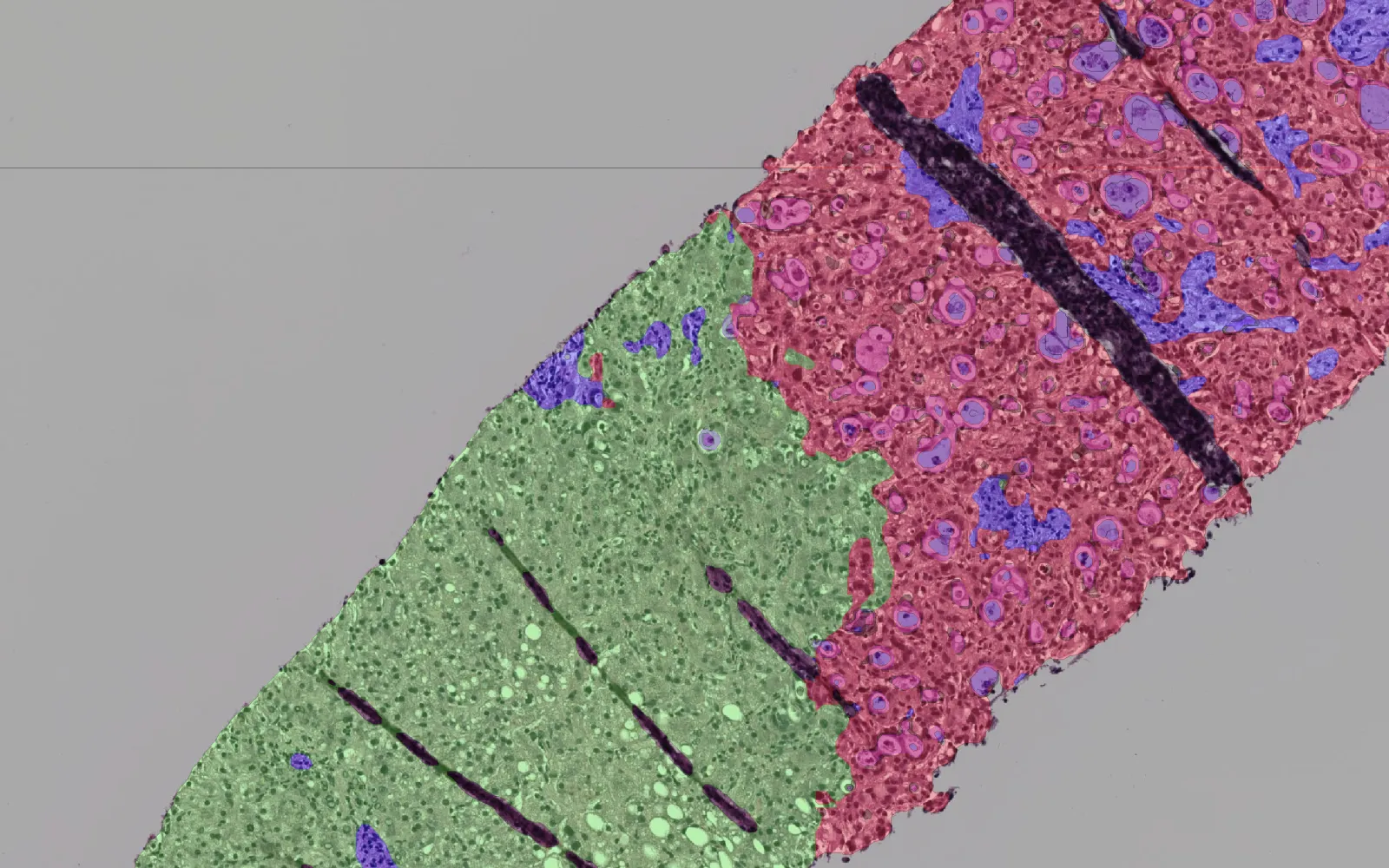
Just as the iconic “little black bag” equipped physicians in the mid-20th century with core diagnostic and treatment tools for house calls, Somatic AI platforms will serve as the foundation for a new era of data-driven, algorithmically enabled care. Portable ultrasound devices enhanced with computer vision and machine learning, like those made by Caption Health (acquired by GE HealthCare in 2023), can guide frontline providers through complex imaging exams while automatically identifying signs of disease. The smartphone in a clinician’s pocket will provide instant access to Somatic AI models of each patient, transforming care from episodic and reactive to continuous and predictive.
Enabling the surgical superhero
The impact of Somatic AI extends well beyond the primary care setting. It will fundamentally transform how specialists approach complex procedures in fields like surgery, interventional radiology, and radiation oncology. The ability to navigate the physical side of procedures and examinations is a key opportunity for Somatic AI. Two DCVC-backed companies, Proprio and Remedy Robotics, exemplify this potential.
Proprio is pioneering a real-time surgical navigation and alignment platform, initially targeting spine and cranial procedures. The company’s core technology, derived from research at the University of Washington’s Sensor Systems Lab, leverages Lightfield cameras to capture rich spatial and depth information from the surgical field. (Lightfield imaging contains the intensity and directionality of all light rays passing through a scene — orders of magnitude more visual information than standard two-dimensional, or 2D, images.)
Proprio feeds these Lightfield streams into GPU-powered deep learning models that construct three-dimensional representations of patient anatomy, track instruments, and enable real-time navigation and alignment. The platform acts as a kind of surgical GPS, guiding the surgeon’s tools and decision-making to sub-millimeter precision. Surgeons can effectively “see” through blood and tissue to visualize underlying anatomical structures, track the position and trajectory of implants, and receive AI-generated alerts about potential deviations or safety hazards. Proprio received FDA 510(k) clearance in 2023 for its technology and is rolling out to leading spine surgical practices, having performed over 50 live and successful surgeries in the first half of 2024.
Importantly, Proprio’s platform is not just enhancing surgical precision and outcomes in the moment but also generating a wealth of data on patient anatomy, surgical techniques, and procedural workflows that can be used to drive continuous improvement across the entire cycle of care. By capturing and analyzing this data at an unprecedented level of granularity and using it to power AI-driven insights and recommendations, Proprio is building a foundation for optimizing everything from pre-operative planning and intra-operative guidance to post-operative recovery and long-term follow-up.
Another key tenet of TechMed is to use Somatic AI to expand and improve care to unserved populations, as we have seen in DCVC portfolio company Remedy Robotics. Today, only 15% of the global population has access to time-critical cardiovascular care. Unfortunately, this care is often marked by imprecision and unacceptably high complication rates. Remedy Robotics, founded by Dr. David Bell, a cardiothoracic surgeon, and Dr. Jake Sganga, a PhD in surgical robotics, is on a mission to provide optimized, complication-free cardiovascular care and make it accessible to all people around the world. Remedy Robotics achieves this by integrating cutting-edge machine learning into the traditionally hardware-driven field of surgical robotics. This approach enables enhanced visualization and precise control of endovascular tools, allowing for the complete remote treatment — and soon, supervised autonomous treatment — of a range of time-critical cardiovascular conditions.
In addition, beyond surgery, imaging, and medical devices, having the ability to continuously (24×7) and remotely monitor and manage patients with at-risk conditions becomes an enormous enabler of TechMed. In the area of Somatic AI, all.health has developed an AI-enabled wearable wristband with a range of sensors, allowing health systems and payors to better manage their patients at risk by detecting serious issues earlier, thus providing better care and lowering healthcare costs — at population scale.
A new paradigm for healthcare — and investors
The rise of Somatic AI represents a fundamental shift in how we approach healthcare innovation and delivery. It challenges us to move beyond the traditional MedTech playbook of incremental device enhancements and embrace a new paradigm centered around data, intelligence, and continuous optimization. New computational insights, built at the intersection of AI and anatomy, will factor into how medicine is conducted.
In this new era, success will require more than just bolting AI onto existing devices or sprinkling in a few software features. It demands a wholesale re-architecting of R&D, commercial, and post-market strategies to put data at the core. The winners will be those who can construct the most clinically relevant and diverse real-world datasets, develop the most intelligent and adaptable algorithms, and deliver the most compelling value propositions aligned with real-world outcomes.
For investors, the rise of Somatic AI offers massive opportunities. But success will require following three general rules:
Of course, realizing the full potential of Somatic AI will require close collaboration with patients, providers, and regulators. Entrepreneurs and investors must work with all these groups to address critical issues around safety, efficacy, data rights, and health equity. Industry and academia should partner on new approaches to validation, from in-silico trials and digital twins to adaptive post-market surveillance. The FDA has taken encouraging steps by releasing its Artificial Intelligence and Machine Learning Action Plan, but much work remains to align regulatory frameworks with the unique challenges and opportunities of AI in medicine.
Ultimately, the rise of Somatic AI represents an opportunity to reimagine our healthcare system around the principles of 21st-century technology — ubiquitous sensing, large-scale data analytics, intelligent automation, and continuous optimization. From wearable devices that detect atrial fibrillation to AI-guided surgical navigation and autonomous catheter-based interventions, it promises to usher in a new era of care that is more preventive than reactive, more personalized than population-based, and more accessible than ever before.
For entrepreneurs, investors, and healthcare professionals alike, the message is clear: the future of medicine lies in harnessing Somatic AI to understand, predict, and optimize human health in unprecedented ways. Armed with these smarter tools and keener insights, clinicians can focus on the most human elements of healing while ensuring every patient receives the highest standard of data-driven, evidence-based medicine.