Remedy Robotics
Vascular intervention without borders
No matter where you live or where you travel, the odds of suffering an ischemic stroke — an interruption of blood flow to part of the brain — are the same. Roughly 700,000 Americans are hit by such an emergency every year, and 270,000 of those people need a catheter-based procedure called a mechanical thrombectomy to remove the clot. But their odds of recovering vary drastically, depending on how quickly they can get to a medical center with a surgeon qualified to carry out the procedure. For every hour of delay, their chances of returning to functional independence go down 20 percent.
Unfortunately, only 30,000 stroke victims each year are able to get an immediate thrombectomy. The problem, simply put, is that there aren’t enough vascular surgeons, and they can’t be everywhere at once. So when we first heard TechMed entrepreneurs David Bell and Jake Sganga talking about how they might be able to fix that, we listened — and we funded them.
This week, the company they started, Remedy Robotics, emerged from stealth after several years of behind-the-scenes R&D to share two announcements. Recently Dr. Vitor Mendes Pereira, a neurosurgeon at St. Michael’s Hospital in Toronto, used Remedy’s N1 endovascular robotic system to perform history’s first fully remote cerebral angiograms — twice from a room 50 meters down the hall, and twice from a different hospital six miles away.
At the same time, Remedy disclosed in an Axios exclusive that it has raised $35 million in seed and series A funding. DCVC led the seed round.
Dr. Pereira’s remote angiograms, which were completed without complications, were a huge step on the way to remote execution of more complex and urgent surgeries such as mechanical thrombectomies. It now seems feasible that a neurosurgeon like Dr. Pereira, guided by live X‑ray images carried over the internet and Remedy’s navigational AI, could save a stroke victim in an underserved area such as Yellowknife or Port Moresby or Kinshasa. As Bell puts it: “We’re giving surgeons superpowers, and we’re putting them in places where they’re not.”
To make Dr. Pereira’s groundbreaking procedures possible, Remedy had to solve several interlinked problems. One was building robotic catheters that could be operated remotely with negligible delay; N1’s latency during Dr. Pereira’s angiograms in Toronto was just 8 milliseconds. Another was finding a way for a surgeon guiding a springy, elastic catheter the whole length of the body (from the groin to the brain, typically) to stay oriented in the 3D space of the body — a challenge even during in-person endovascular surgery, given that surgeons are typically watching a flat, 2‑D X‑ray fluoroscopy image in which the blood vessels themselves are invisible.
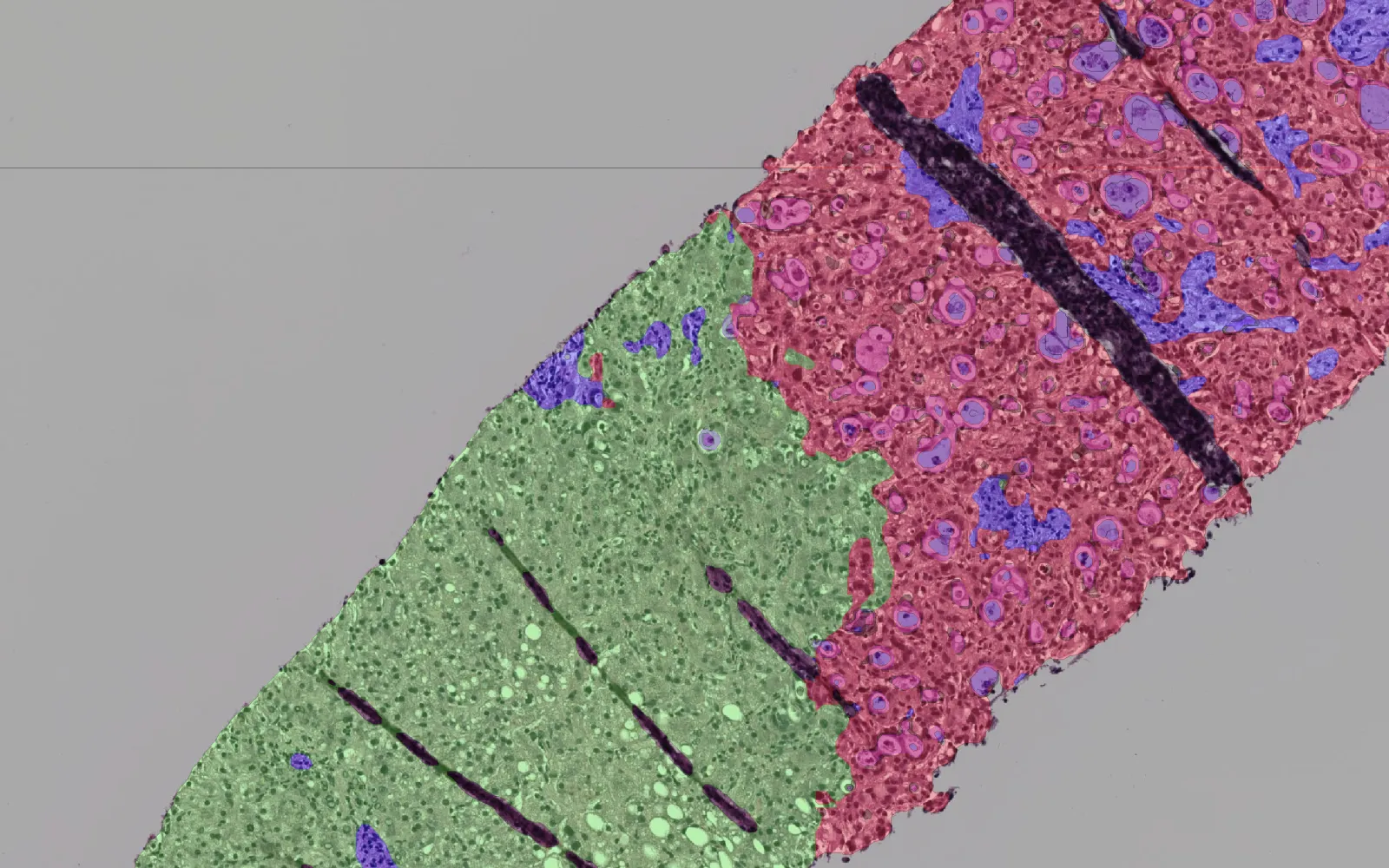
Remedy approached the second problem using machine learning. Every stroke patient gets a CT or MRI scan, and in theory this 3D data could help guide endovascular surgeons as they rush to reach and remove a brain clot. The problem is that the human spine, shoulders, and skull are bendable, making it difficult to overlay this 3D data on a live 2D X‑ray image and keep them aligned.
Remedy collected a huge dataset of chest, neck, and head scans, hired humans to label the main anatomical landmarks such as blood vessels and vertebrae, and used that data to train algorithms to recognize the equivalent features in CT or MRI scans. That allows N1’s software to accurately superimpose 3D reconstructions of a patient’s anatomy onto the X‑rays, which in turn helps surgeons guide catheters around tight corners. On top of that, Remedy came up with a system of fiducial marks on the catheters themselves that the software can use to show the surgeon how the catheter is oriented (downward into the plane of the X‑ray, for example, or upward out of that plane).
“I always thought it was crazy that we have all this 3D data from a CT scan or an MRI and then we go do the procedure blind to the third dimension,” Bell says. “But because we can now do all that cool stuff with reconstructing the vessels, we start to be able to do all of these procedures in simulation, before the case even starts. The goal here is to do all these procedures in software before the patient even gets on the table.”
There are about 3,500 hospitals in the United States with catheterization labs that could support the N1 robot, Bell says — but only about 300 with stroke specialists. Remedy’s first aim is to make cerebral angiograms and thrombectomies safer and faster at hospitals that already do them. Then it will seek regulatory approval for remote stroke surgery, both in Australia and the U.S. (The company eventually plans to use the technology to treat 30 different cardiovascular conditions, including problems like stroke and traumatic bleeding that require immediate remote care and elective conditions such as subdural haematomas and unruptured aneurysms that could be treated more quickly and safely.)
Remedy is using its seed and Series A funding to grow rapidly, hiring best-in-class TechMed engineers, software developers, and clinical trial managers. “Surgical robotics has been such a slow-to-innovate and hardware-focused field,” Bell says. “The machine learning component is really what makes this possible. And it’s not just for stroke — it’s a bunch of endovascular conditions.”
We’re confident that this new generation of AI-powered robotics will profoundly improve patient outcomes — and we’re proud to support Remedy in its pioneering work.